Class News
My Telltale Heart
by Bob Kaiser
The Washington Post
Feb. 29, 2004
Click here for an interactive graphic
It's a horror story, all right. One moment, your life is normal ― endless. The next, a surgeon saws open your chest, freezes your brain and scrambles to keep you alive, literally holding your heart.
WHEN I AWOKE LAST MARCH 26, I saw the same old me in the mirror, the paragon of good health I'd been seeing for decades: in fine shape, thanks to regular racquetball, fitness machine workouts, yoga and outdoor activities; no bad habits; healthy parents, then nearly 90 years old. In 12 days I would be 60, a milestone in what had always seemed to be a charmed life.
My mistake. I was confusing the habitual with the perpetual.
On that Wednesday in March the habitual crumbled. After a good early-morning yoga class I was in my bathroom when I felt a sudden, ominous thumping at the top of my chest; tingling and weakness in my left arm; blurred vision in my right eye.
Luckily, my wife of 38 years was at home, and I called out to her. She telephoned my doctor, Robert Hardi, who had given me his cell phone number a few years earlier, for which I was suddenly very grateful. He answered at once, and told Hannah I should lie down. If the symptoms did not disappear in 10 minutes, he said, she should take me to the emergency room at Sibley Memorial Hospital in Northwest Washington.
Ten minutes brought no relief. We got in the old Jeep Cherokee and drove from our Dupont Circle townhouse to Sibley, five miles out Massachusetts Avenue. The symptoms got stranger along the way. In front of the Islamic Center mosque at Rock Creek Park my right eye saw only bright light, no shapes or colors. Scary.
But not terrifying, curiously. Some protective mechanism stopped me from thinking about what these symptoms might mean. I was comforted by the thought that I was fully conscious and would soon be at the hospital. Things were under control, sort of. My best friend was driving, she seemed calm, I had no real pain. There was no panic.
Late morning is a good time to arrive in an emergency room. Business is light. I was quickly registered and put on a gurney, then zippered into my own space behind curtains, known in the Sibley ER as Room 9.
Sibley's chief of emergency medicine is Andrew Sumner, 57, a round, soft-spoken Georgian. He took the job at Sibley in 2001, he told me later, as a way to take it a little easier after years spent closer to the front lines of urban emergency medicine in Baltimore. There he practiced at the Johns Hopkins and Good Samaritan hospitals, and taught emergency medicine at Hopkins. In Baltimore, gunshot wounds, drug overdoses and other manifestations of urban poverty and mayhem were common. At Sibley, a comfortable hospital just off MacArthur Boulevard in a leafy, well-to-do part of Northwest Washington, a more typical visitor to the ER had cut a finger chopping onions, or was having a heart attack after years of heart disease.
Months later, when we could have a relaxed conversation about the morning of March 26, Sumner confessed that his first hypothesis that day was ― an anxiety attack. "I was thinking to myself, blurred vision, numbness in the hand, funny feelings in the chest ― this is mostly anxiety," he recalled. "Then you went on to tell me about your yoga class that morning . . ." In other words, he thought I was an overanxious New Age type.
But this hypothesis did not deter Sumner from looking further. "I stood you up and I had you put your palms out flat. This is a test of subtle motor weakness. Your ring finger and little finger were curled up on your left hand [often a sign of stroke or something else wrong in the brain]. When I saw that, I knew immediately that something was wrong . . . I quickly went from thinking that you're having an anxiety attack to thinking something bad is happening here . . . It was like the light came on, and I said, 'Oh, no.' " Sumner listened through his stethoscope for a telltale sound in the carotid arteries of the neck, which carry blood from the aorta just above the heart to the brain. He didn't hear what diagnosticians call a "bruit," a swooshing sound that can signal a blockage, but he did hear a troubling, harsh sound. He took me downstairs for an ultrasound examination of the two carotid arteries. It showed that the inner layer of one of them had separated ― or "dissected" ― from the outer two layers, partially diverting the normal flow of blood to the brain into a kind of pocket. When a carotid dissection blocks the blood flow, death or a stroke can follow, though some carotid dissections are not so serious.
Sumner started to walk back upstairs to tell Hannah the news. And then he stopped. A far more frightening possibility popped into his mind. Maybe the problem in the carotid artery was not cause, but effect ― the result of a dissection that began in the aorta.
Dissections of the aorta are extraordinarily dangerous. The aorta is the body's primary artery ― really an extension of the heart itself. If it fails, the brain and body get no blood. Actor John Ritter died of an aortic dissection last September.
Sumner had never seen dissections of the carotid or the aorta in his own practice, but he knew about both. For years, he has augmented his income and his experience by appearing as a witness in medical malpractice suits. As a witness Sumner had reviewed one case of carotid dissection, and several cases of aortic dissection ― cases he remembered that morning, walking up the stairs.
A chest X-ray taken soon after I arrived at Sibley showed a normal aorta. But Sumner now remembered that "about 25 percent of aortic dissections have normal chest X-rays. So, rather than go talk to your wife, I turned around and went to see [Sibley's] chief of radiology, Dr. Richard Newman."
Newman recommended a spiral CT scan of the chest. By injecting me with contrast dye, then taking pictures of cross-sections of my heart and aorta, the doctors could now see what the chest X-ray did not reveal.
"We got these beautiful pictures, showing an aortic dissection beginning at the root of the aorta and extending into your carotid arteries," Sumner recalled. "I thought, this is one hell of an anxiety attack! You've transferred your anxiety over to me now."
Unless repaired, dissections of the ascending aorta kill most of the people who have them, instantly or eventually. The risk of death for those who survive the dissection itself rises sharply as time passes ― about 1 percent per hour for 48 hours. The tests at Sibley had already taken three hours, and they began nearly an hour after my first symptoms. My chances were ticking away.
The aorta is shaped like a walking cane. The "handle" end rises out of the heart 3 to 4 inches to the top of the chest, where the carotid arteries branch off to the brain. When the inner layer, or intima, of the aorta dissects, it separates from the artery's other two layers, and often tears. A violent dissection can literally rip the carotids off where they attach to the aorta, causing instant death. A milder dissection creates a "false" channel, or pocket, into which the blood flows. This is what Sumner and Newman saw in those "beautiful" pictures.
My dissection misdirected some blood into a false channel, but left an
opening for the normal channel for circulation to the rest of my body.
Sometimes, however, the false channel takes all the blood that the heart
can pump, quickly creating a dangerous dead-end. Under continuing pressure
from the beating heart, the aorta can rupture, flooding the pericardium,
the protective sac that surrounds both the heart and the aorta. The heart
cannot beat in a pericardium suddenly filled with blood ― again, instant
death.
In my case, some natural defense mechanism in my body was activated at
this moment of crisis that gave me further protection. Normal blood
pressure, measured in two numbers, is 120 over 80. My own blood pressure
was typically a little higher, about 140 / 85. But on the morning of March
26, when a nurse took my blood pressure at 11 a.m., it was 77 / 54. My
pulse, usually 65 to 75 beats per minute, was 56. For the next five hours,
these low readings hardly changed.
This, literally, was just what the doctor ordered. Medical texts instruct emergency doctors to treat an aortic dissection with medications to lower the blood pressure and pulse rate, to reduce pressure on the aorta wall and avoid more damaging tears. But my body didn't wait for medication. It did this on its own.
"It was kind of like God was smiling that day and wanted you to make it," Sumner said later ― not exactly a scientific explanation. He also offered another theory: Though I had some bad genes that contributed to the dissection, I also had some good ones, which gave me excellent cardiovascular health outside the aorta, and I was generally in good shape, making it easier for my body to protect itself.
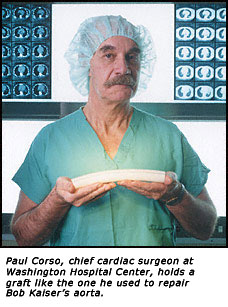
When Sumner reached his final diagnosis at 3:04 p.m., my survival was by no means assured. I needed surgery immediately. Sumner called the heart surgery group at the Washington Hospital Center, his first choice in a cardiac emergency. When Paul Corso, the chief cardiac surgeon there, heard Sumner's account, he said he would send a helicopter to pick me up, and would operate as soon as I arrived.
Now Sumner returned to the emergency room, where my wife was waiting, to give her the bad news. At the same time, our friend Janice Downie, who lives near Sibley, arrived in the emergency room to be with Hannah. Sumner took them both downstairs to tell me about my situation. Hannah and Janice both remember the conversation as deeply shocking. I don't remember it at all. Sumner had given me a calming drug, Ativan, and a painkiller, Toradol. I was mellow. I remember very little that happened after I took them.
Sumner began by saying this was perhaps the worst day of my life. He told Hannah that "your husband could die at any moment." But he also said there were better possibilities: Aortic dissections can be surgically fixed, and I would be going to an excellent surgeon, fast, by helicopter. I have a vague memory of anticipating my first helicopter ride since the Vietnam War. And then nothing happened. The helicopter did not arrive. I lay there. Hannah and Janice nervously checked every few minutes with a nurse ― where's the helicopter? After about 45 minutes someone told them the wet, blustery weather made it impossible to fly. So the hospital center had sent an ambulance. We had no choice but to wait for it. Sibley has no ambulance of its own, and Sumner said there was no point in calling a D.C. ambulance, since they usually refuse to transport patients from one hospital to another, on the grounds that they are already in a hospital.
The Washington Hospital Center ambulance finally arrived at 4:22 p.m. Two
young men bundled me into the back of the truck. Hannah rode in front; a
technician who was monitoring my vital signs rode with me. Rush hour was
just beginning as we set off on the nine-mile trip. On Military Road the
traffic was suddenly heavy. Shouldn't you use the siren, Hannah asked the
driver. It's up to the man in back, the driver responded. The technician
had already made clear his concern about a bumpy ride ― I needed to be
kept as still as possible. But now he agreed to use the siren, and the
driver pointed his ambulance into the oncoming lane. He never drove fast,
but with the siren blaring and lights flashing he could drive steadily,
without stopping.
When we arrived at 4:50, Dr. Corso was waiting. Hannah was struck by the
relaxed atmosphere in the emergency room. It felt a little like a cocktail
party, she remembered later. Corso seemed more like a cordial host than a
surgeon who was about to save her husband.
Months afterward I asked Corso about this. The apparent calm was deliberate, he said: "No one wants to see a surgeon coming out there who looks in a panic." In fact, intense preparations had begun. The operating room was being prepared. Blood was taken and tested.
Paul Corso is 59, tall, slim and erect. What hair he has left is mostly white. He compensates, as he puts it, with a handsome, thick mustache, which matches two bushy eyebrows. He studied medicine at George Washington University and surgery at GW Hospital. But he almost studied airplanes and flying, he later told me, which seems eerily appropriate for a cardiothoracic surgeon. The CT surgeons are known to their colleagues as the top guns of the surgical profession. They routinely take on life-and-death procedures as though they were, well, fun.
Presenting his plans for me to Hannah, Corso was crisp and confident. He didn't talk about the possibility that I could die at any moment, nor did he reveal any anxiety about what he was about to do ― he had done similar operations more than 200 times. I heard his explanation, too ― I've seen my signature on a permission form authorizing him to cut me open. But I have no memory at all of signing the piece of paper.
I was on the operating table at 6:30 p.m. When he saw the computed tomography (another CT) scan, which had come in the ambulance with me, Corso said later, he saw grounds for hope that my dissection was limited in size and seriousness in ways that would allow a relatively simple repair. At the same time, he had an entire artificial aorta ― an "elephant trunk," the CT surgeons call it ― ready in case the damage to mine was greater than he expected. "You never know how complex it's going to be until you get in there," he said later.
I was put to sleep and laid out on an operating table that tilts in all directions. For this operation, Corso puts the patient on his back, and tips the head down and the feet up. This posture reduces the chances of air bubbles in the bloodstream rising into the brain.
Corso began at 6:35 p.m. by sticking things into my body: a breathing tube down my throat to force air into my lungs; a catheter tube through a big vein in my neck and into my heart to monitor pressure, blood flow and temperature; another finger-size tube down the throat into my stomach to take continuous echocardiograms that would allow the operating team to "see" everything in the center of my body, from my esophagus to my stomach.
Using those devices, Corso then made an inside-out inspection of the damage. No visible surprises. Nurses then prepped me with a Betadine solution from my ankles to my chin, shaved a lot of body hair and got me into position. Corso began.
The first cut was into my groin to put a tube into the femoral artery, which would receive blood from the heart-lung machine during much of the operation and circulate it backwards through the body. Next he carved open my chest, beginning two inches below my Adam's apple and continuing 8 3/4 inches toward my navel ― first with a knife, then a reciprocating electric saw that cut up and down through the sternum, the flat bone in the middle of the chest that is about 3/4 inch thick. Cutting it open took no more than 10 seconds, though the scar this created will now last as long as I do.
"The chest muscles come in and attach right at the midline of the sternum, so we go right between those muscles; we don't cut muscles," Corso explained. "Then we have a retractor that pulls the sternum open . . . Then there is fat that covers the sac the heart's in. We free that up and cauterize that, and open the sac . . . to evaluate what's going on."
He quickly saw that my aorta was enlarged and bruised in the area just above the heart, where the dissection was occurring. Now Corso needed to open the aorta, but he could not do this as long as it continued to carry blood from my heart to my body. Repairing a working aorta would be like trying to patch a high-pressure water main while it remained in use. Corso would have to shut down the circulatory system.
This would require the heart-lung machine and deep hypothermia, two modern medical miracles about which I knew essentially nothing before they helped save my life. In crude terms, deep hypothermia and the heart-lung machine allowed Corso to put my body, including the heart and brain, to sleep for 32 minutes. For the first time in 60 years, neither of those vital organs did anything, and the rest of me existed in a kind of suspended animation. An electrocardiogram (EKG) during those 32 minutes would have reported no heart function. An electroencephalogram (EEG), which measures brain waves, would have shown none.
When Corso first told me this, five months after the operation, I was taken aback. "So in what sense," I asked, "is one alive? If your brain and heart are both suspended in this way?"
"If your definition of life is based on electrocardiogram and the EEG," he replied, "you're dead."
"But I was still breathing?"
"Well, no, you're not breathing. You're paralyzed. Nothing's happening. Now, we know that you're not dead. We've created this situation. The cells are kept alive, they are alive, they're just not making electrical noise. Once you've warmed back up and we bring you back to normal, then, obviously, [the heart and brain] work again . . ."
Except during the critical 32 minutes, when nearly everything was stopped, the heart-lung machine did my breathing for me. This is the apparatus that makes modern open-heart operations like mine possible. To oversimplify, the machine sucks "blue," deoxygenated blood through a tube from the right atrium of the heart and directs it across the fine surfaces of the device. The machine delivers oxygen as the blood passes over the interface, and the blood cells absorb it, as they normally do in the lungs. The oxygenated blood can then be pumped back into the body.
The heart-lung machine also has a refrigerator-like coil that chills the blood, creating deep hypothermia. A body in deep hypothermia remains in a sort of super-cooled suspended animation during the critical phase of the surgery. The machine cooled a quantity of my own blood down to 50 degrees ― 48.6 degrees colder than normal. The cold blood was pumped very slowly into my brain. It came in backwards, through the superior vena cava, the vein that ordinarily returns blood from the brain to the heart. After completing its backwards journey through the brain, providing the oxygen the brain needed to survive, the blood dripped through the carotid arteries (ordinarily the suppliers of blood to the brain) into the arch of the aorta.
The arch of the aorta is the top of a loop, but because I was almost upside down on the tilted operating table, it was now the bottom, and could trap the deoxygenated blood until a plastic tube returned it to the machine for re-oxygenating, re-cooling and re-circulation through the brain.
The cold blood that preserves the heart during the surgery doesn't have to circulate. Instead it is exchanged for a new batch about every 20 minutes. During heart transplant operations, hearts are kept alive this way for up to three hours.
What, I asked, did Corso do while I was, literally, chilling out on the operating table? "We're just standing around, listening to the radio," he replied ― usually smooth jazz or classic rock-and-roll.
In deep hypothermia, with blood circulation (except through the brain) at a standstill, the aorta became just an empty pipe, and Corso could cut into it to explore further. "Because I didn't know where the tear started," he explained later, "I just opened it anywhere, just to sort of get in there and start looking around."
The naked eye, and a surgeon's magnifying viewer, was all he needed to confirm the dissection just beyond the aortic valve, next to the heart. Exploring farther, he found a tear about an inch and a half long farther along the inner wall of the ascending aorta. This is where the blood got in between the layers of the aorta to create the dissection. But the lining of the aorta's inner wall outside these two areas seemed relatively healthy. When repairing other dissections, Corso said, he has found that this lining was shredded "like wet tissue paper."
So far, it was all good news. Corso decided the operation could proceed along the lines he had initially envisioned. He amputated the aorta just above the heart. Now he could see everything inside. In the upper part of the aorta, he decided to stitch the tear, and to close and seal the false channel it created by injecting BioGlue. This is a miracle product made from a cow protein and a designer chemical that dries to the consistency of soft rubber. BioGlue is not permanent, but it gives the body's own regenerative powers a chance to go to work.
This first phase went well. "We now had an intact aorta, no obvious dissection anywhere, it's well fixed."
Next Corso measured the bruised area of the "proximal" aorta, the section closest to the heart where the most serious dissection had occurred. He decided to replace a three-inch section with a size 28 Dacron graft, a grooved tube 28 millimeters, or about 1.1 inches, in diameter, made of knitted Dacron velour. This material is used because the body seems to like it; blood platelets quickly line the inner layer, making it look and behave like a human blood vessel, while other cells surround it on the outside. In just a few weeks, the Dacron graft is covered, inside and out, with the patient's cells. Corso stitched one end of the graft to the upper part of the ascending aorta.
Next he had to decide whether the dissection had so damaged the aortic valve that it would have to be replaced. The aortic valve consists of three leaf-like cusps that open with each heartbeat to allow blood to pass from the left ventricle, the heart's main pumping station, into the aorta. Normally, the inner wall of the aorta holds the valve in the proper alignment, but the dissection had allowed it to droop, so it leaked. Corso thought he could "re-suspend" the valve with a few well-placed stitches that would restore it to proper alignment. After putting in those stitches he poured a little water on the valve to make sure it had stopped leaking. It had.
All that remained was to stitch the base of the graft to the remaining bit of original aorta, just above the valve. Now I had a reconstituted aorta, ready for use. Slowly, Corso and his assistants brought me off the heart-lung machine. They warmed my blood back to 98.6 degrees. My heart started to beat again on its own, prompted into action by the warm blood's effect on the heart's own internal pacemaker.
"I had your heart in my hand," Corso recounted. "I could feel how well it was squeezing."
The operation had taken 4 hours 42 minutes. At 11:20 p.m. Corso could go out to the waiting room to tell Hannah and our daughter Emily, 28, that the operation was a success. Almost giddy, they were soon on their cell phones reporting the good news to daughter Charlotte, 30, and other family and friends.
I was "a bad patient," as Dr. Corso put it when we had our first real conversation about the operation several weeks after I left the hospital. In the days after the operation I was obstreperous, and kept trying to pull the tubes out of my body. "We couldn't orient you," he said. Usually, he explained, a patient knows in advance what the effects of his open-heart surgery are likely to be, so he isn't surprised by what occurs. They didn't have a chance to brief me, he said.
For nearly a week after the operation I was out of it: sedated, bloated, uncomfortable, dependent on oxygen pumped into me through a mask. My wife and daughters found me a rather pathetic and often terrifying sight, sometimes shaking like an aspen leaf, unable to speak, kept alive by numerous tubes coming into and out of my body. My ankles were so swollen they disappeared. I rarely opened my eyes or moved for several days. My complexion was yellow. The doctors and nurses kept telling Hannah everything was fine.
And slowly I got better. On March 29, three days after the operation, Hannah reported that when Emily told me it was 5 o'clock in the afternoon, I announced that "the sun has passed over the yardarm." (It would be months before I made good on that old saying and had my first cocktail, however.) On the same day, I allegedly told an attractive blond nurse that she was "a sight for sore eyes." I remember none of this. During the first week I was actually tied down in bed.
My first memory, I think, is of a nurse telling me in a loud voice: "Mr. Kaiser, you cannot do that. You CANNOT do that! You have had serious open-heart surgery, and you simply cannot do that!"
I don't remember what "that" was, and I don't remember a face, just the voice. But I do remember thinking I was in some kind of dream. I knew something had happened to me; I must have understood that I was in a hospital. But open-heart surgery? That made no sense. My healthy 90-year-old parents had no heart trouble, nor did any of my relatives. So how could I have needed heart surgery? Obviously I was dreaming.
Doctors came often, and they must have kept telling me what had happened. I remember being told several times that I was "a very lucky man." Slowly, all this talk began to sink in. Hannah remembers standing beside my bed in the ICU on March 30. I took her hand in mine and said, "Dr. Sumner saved my life."
As the sedation was reduced, I began again to pay attention to my surroundings. I wanted to read the paper, but I was still too weak to muster the energy and focus, so my wife and daughters read aloud to me, a great pleasure. Hannah brought a boombox to my room, so I could listen to Mozart, and to NPR. According to Hannah, I interviewed every nurse and technician who came into my room about my situation. The war in Iraq was beginning ― I was missing a big story. I resolved not to be bothered. The war was big news, but in my life, it would not make the front page.
As I got better I had to absorb the thought that I had "dodged the Reaper," in the wonderful phrase of John Bigelow, a friend since high school and author of one of the many cheering e-mails I received during those days. This was hard; at first I thought a near-miss like this could create real psychological problems.
I had nearly died because of an ailment I didn't know I had ― indeed, probably could not have known I had. Corso said later that if he had used the magnetic resonance imaging (MRI) machine, the best "eyes" modern medicine has to see inside the body, to look at my aorta just 10 minutes before my dissection occurred, "it probably would have shown nothing."
At first the mind reacts to trauma reflexively. My reflex was to think
about future writing projects. While still in a drugged state,
sleep-deprived by the ICU routine that involves constant waking, noise and
disruption, I asked Hannah to let me use her laptop computer to make a few
curt notes.
The first one said: "You just saved my life, and what am I going to do
about it? Write a newspaper article? Isn't that slightly ridiculous?"
This was a reference to the article you are reading. I decided in those
first days in the hospital that I would try to write about how Drs. Sumner
and Corso saved me. I also wanted to say, in print, what attentive care I
received from everyone at Sibley and the Washington Hospital Center. Then,
as now, this seemed like a small, perhaps feeble gesture, but writing is
what I do.
Only later did I realize that by devoting my daydreaming time almost
compulsively to writing projects, I was, I think, asserting my
determination to resume my professional life. I may have had a close call,
but I did indeed dodge the Reaper.
I returned home on April 6, the day before my 60th birthday ― the beginning of the rest of my life, a cliché that suddenly had new meaning. Virtually everything suddenly had new meaning, beginning with "family" and "friends." These two had come through for me in the most profound way during those 11 days in the hospital. Once I had really regained consciousness, Hannah read scores of e-mail messages from friends and colleagues, and they had the effect of a fine tonic on my spirits. I could sit for 45 minutes listening to her read cheerful, affectionate messages, and feel physically better when she finished. Don't ever wonder if you should write to a friend in the hospital; just do it.
Being home without the hospital center nurses was hard, particularly on
Hannah, who had to feed me, wash me, give me my many pills, help me dress
and much more. After open-heart surgery the lungs are almost invariably
bruised. The body has been cut up like a salami; many wounds have to heal.
The beta-blocker drugs ― which slow pulse and lower blood pressure to
spare the healing aorta ― left me dizzy, short of breath or just
exhausted.
Nine days after I got home I took a shower. Hannah stood right beside the
tub to be sure I didn't fall. Suddenly she saw the left side of my face
lose all its shape and movement. I realized my left arm had lost most of
its strength, and speaking was difficult. I was having a mild stroke. I
was in the same bathroom I'd been in when I sensed the first symptoms of
my dissecting aorta just 20 days before ― here we went again.
This time Hannah called Ramin Oskoui, the cardiologist to whom Corso had entrusted my care as I was leaving the hospital. Oskoui, 39, a former varsity soccer player at Georgetown, told Hannah to take me back to Sibley, and, to our pleasant surprise, he was there to meet us. Again we remained calm on the drive out Massachusetts Avenue.
Strokes after surgery like mine are not rare. As several doctors later
explained, stitches and patches in the aorta leave rough spots. Blood
platelets can form small clots around these spots, and they can break
loose and move up the carotid arteries into the brain, causing a blockage
that constitutes a stroke. This is probably what happened that morning.
So I had another five days in the hospital. The neurologists quickly
concluded that the stroke was very minor, and that its effects would be
mostly short-lived. The weakness in the left arm disappeared almost
immediately. Ten months later I have only a slight numbness around the
left corner of my mouth and at the root of my tongue to remind me of the
stroke.
Dr. Corso typically invites his patients to see him for a final conversation shortly after surgery. My meeting was postponed by my stroke, but I went to see him on April 22. This was a big moment for me, I think because I was anxious for reassurance that I really would recover from the two roundhouse punches I had absorbed.
"You had a serious problem," he said, using words I have repeated to friends many times since. "We fixed it."
He told me something else just as important: When I came into his
operating room on March 26, neither Corso nor I knew that there was a
history of aortic disease in my mother's family. My uncle Sam Greeley, my
mother's youngest brother, had an aneurysm in his aorta in 1982, when he
also received a Dacron patch from a surgeon in Milwaukee. (He's now 77 and
doing well.) I only learned this history when Sam was visiting his sister,
my mother, shortly after my operation. He recounted this story, then
explained that his mother, the sister of my maternal grandmother (my
grandfather married two sisters sequentially, a story for another
occasion), had died, at 82, of a ruptured aorta.
Three cases in one family persuade the experts that I had inherited a
congenital defect in the connective tissue of my aorta. Researchers at
Cornell University have now taken on my entire family as part of a study
to try to figure out the genetics of "family aortic aneurysm disease."
If mine was a genetic defect, Corso said, "then what happened to you on
March 26 could have happened on any day since your 40th birthday."
Any day in the last 20 years?
This was harrowing, but ultimately helpful, news. My passport would show that in those years I had traveled throughout Western Europe, in Russia and across Siberia, to China, Indonesian Borneo, Uzbekistan, Kazakhstan, Tajikistan, Slovakia, Romania, Bulgaria, Chile, Brazil, Argentina and several other exotic places. Few if any of those countries have the doctors or facilities to deal with an aortic dissection; if struck in any of them, I probably would not have returned.
This conversation profoundly altered my sense of what had happened to me. Initially I felt that my aortic dissection had ended my charmed life ― my luck had run out. Corso's words upended that conclusion. If the dissection was caused by an inherited genetic flaw over which I had no control, and if the dissection occurred when I was perfectly positioned to get speedy, successful treatment and a repair that could last for 20 or 30 years (which Corso also predicted), where was the bad luck? No, I had to conclude, this was another example of my charmed life.
Everything about my aortic dissection, down to the excellent prognosis the doctors now give me after the final healing of my carotid artery and the total success of all the other repairs, was an example of good luck. It starts with the insurance card in your wallet. If you have to suffer an aortic dissection, try to do it with good health insurance ― it's expensive (more than $120,000 in my case). And luck should bring you to the emergency room in the late morning, when the chief of emergency medicine is free to take on your case himself. He should be a creative practitioner who is familiar with aortic dissection ― one of the most misdiagnosed medical crises in the lexicon. Everyone should be so lucky.
Daughter Charlotte's wedding to Nick Peterson on May 10 was wonderfully
timed. Of course it was unfair to Charlotte and Nick to have the ghost of
the dad who almost wasn't there hovering over the event like a cloud. But
they were forgiving, and for the dad who was there, who could give a toast
and embrace the guests, it was a glorious spring day, literally and
figuratively.
The May sun was warm and spirits were high. For me it was a day of great
promise. I could dream of grandchildren and a second daughter's wedding
someday ― even of a big-league baseball team in my home town. I could
dream of a future that had almost eluded me entirely. And there have been
many more glorious days since, days that are memorable not because of any
fame or fortune, but just because they happen.
When friends now ask what lessons I learned from this adventure, my first answers are hardy perennials: Seize the day, appreciate the ordinary. Wisdom or just cliché, the label does not alter the satisfaction I can now take from a wife's smile, a daughter's tease, a friend's hug, the angular light of a bright winter sun in an infinite blue sky.
An acute Type A dissection of the ascending aorta has killed many. It nearly killed me ― but it didn't. How sweet it is to type those words.
Robert G. Kaiser, an associate editor of The Washington Post, is a native Washingtonian who, during a 40-year career at the paper, has covered the Vietnam War and the Cold War in the Soviet Union, and has served as managing editor.